Introduction
Hematopoietic stem-cell transplantation (HSCT) has demonstrated only curative potential for patients with myelodysplastic syndrome (MDS), still prognosis after HSCT are highly different in MDS patients. Over the past decade, several studies have demonstrated that outcomes after HSCT are influenced by clinical and molecular factors, which suggests that a prognostic model combining clinical and molecular-related factors are needed to be identified.
Method
A total of 138 MDS patients who underwent allogeneic HSCT between 2010 and 2018 at the Institute of Hematology and Blood Disease Hospital were considered for inclusion in this study. Median follow-up duration was 33 months. A Custom Amplicon panel targeting exons of 185 genes was used for deep sequencing before transplant. We used a LASSO Cox regression model to achieve shrinkage and variable selection from prognostic factors (P<0.1 in log-rank tests) to build risk score for predicting overall survival. A nomogram was constructed to display the risk of death in individuals. The discrimination of the risk score was measured by the concordance index (C-index) and areas under time-dependent receiver-operating characteristics (ROC) curves (AUCs), and the calibration of the risk score was explored graphically by calibration plots. Patients from the whole cohort were randomly assigned into a training group comprising two-third of the patients, and validation cohort, comprising the remaining one-third of the patients.
Results
In our cohort, U2AF1 was the most recurrently mutated genes (31%), followed by ASXL1 (23.9%), RUNX1 (14.5%), TP53 (10%) and TET2 (10%).
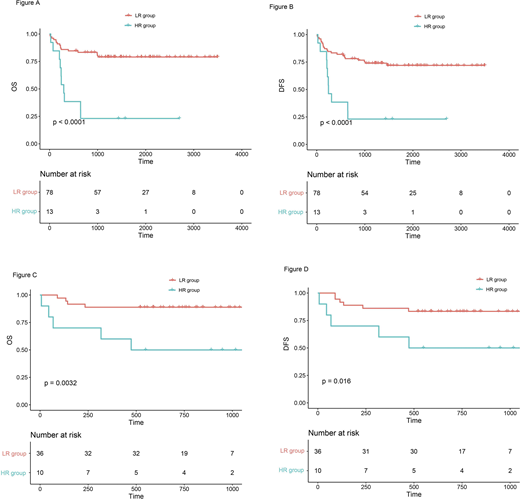
Univariate analyses in training cohort shows, HCT-CI≥3, Blast>0.065, IPSS-R score, TERT, ANKRD26 and PDGFRB mutations were significantly associated with poor OS (P < 0.05). Five variables were incorporated in our scoring model by LASSO, including IPSS-R score, HCT-CI, TERT, PDGFRB, ANKRD26 mutation. A risk scoring model was developed incorporating the weighted coefficients of these variables. The risk score grouped patients into two subgroups: low risk (LR, score ≤1.7, n= 78) and high risk (HR, score > 1.7, n= 13) groups. The 3-year OS for LR and HR groups were 80.5% and 23.1% (P < 0.0001), and 3-year DFS were 73.9% and 23.1% (P < 0.0001), respectively (Figure A-B). The similar results were also observed in validation cohort (3-year OS 88.9% vs. 50.0%, P= 0.0032; 3-year DFS were 83.3% and 50.0%, P =0.016, Figure C-D). Concordance index [train: 0.682, 95% CI (0.63, 0.734), validation: 0.747, 95% CI (0.655, 0.839)] demonstrated well discrimination power and calibration plots showed that the nomograms did well compared with an ideal model.
Conclusions
Here we create a new model combining clinical and molecular-related factors provides better survival stratification for patients with MDS receiving HSCT, provide a useful tool to predict transplant outcomes for MDS patients before transplant. This could have important implications as it can help better identify MDS patients who will benefit the most from transplantation, and may impact the choice of intensity of preparative regimens for transplantation as well as post-transplant maintenance therapy. Additional independent cohorts and prospective studies are needed to externally validate our model before implementation into clinics.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal